III期试验表明,用放射外科治疗脑转移灶4个以上的患者,减少了认知能力下降且不影响生存
时间:2021-02-18 作者:盛诺一家
一项新的随机III期临床试验(NCT01592968)结果表明,立体定向放射外科治疗应替代全脑放疗作为具有4个或以上脑转移灶的患者的治疗标准。相比全脑放疗,高度集中的立体定向放射外科治疗导致了较少的认知能力下降,并取得了同等总生存期。
该研究的第一作者、德克萨斯大学MD安德森癌症中心的放射肿瘤学副教授和脑转移医学中心联合主任Dr. Jing Li说:“这项研究提供了强有力的证据支持用更集中的放疗替代全脑放疗来治疗有多个脑转移灶的患者。”
“很长一段时间以来,全脑放疗一直是治疗脑转移灶的主要手段。然而,当立体定向放射外科治疗变得可用时,我们看到它有潜力减少全脑放疗相关的认知退化并改善患者的生活质量,”Dr. Li表示。立体定向放射外科治疗对患者来说更方便,能最大程度地减少全身治疗的中断,通常在一天时间内完成,而全脑放疗通常需要在两周时间内进行10次治疗。之前的研究将立体定向放射外科治疗确定为具有1-3个脑转移灶的患者的治疗标准,该试验是在此基础上开展的。
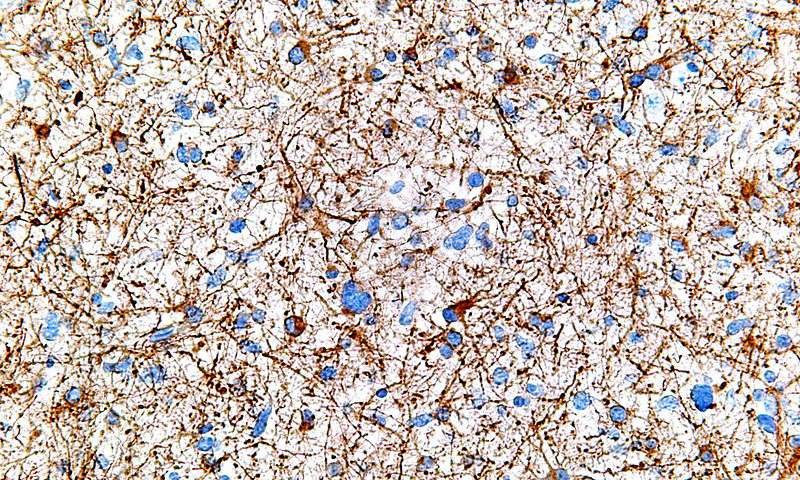
在这项随机III期试验中,MD安德森的放射肿瘤科医生对72名成年患者进行了治疗,他们具有4-15个未经治疗的非黑色素瘤脑转移灶,其中36人接受了立体定向放射外科治疗,余下36人接受了全脑放疗。全脑放疗组患者也被推荐使用memantine,这是一种用于治疗痴呆的处方药,因为另一项III期试验发现,该药有助于延缓接受全脑放疗的脑转移患者的认知能力下降。研究人员通过学习和记忆、注意力持续时间、执行功能、语言流畅性、处理速度和运动灵活性等标准测试来追踪患者的认知功能。
与全脑放疗组患者相比,立体定向放射外科治疗组患者的认知功能得到了更好的保留。放疗后4个月,立体定向放射外科治疗组患者的记忆功能测试得分高于其基线得分。全脑放疗组患者的记忆功能测试得分较基线更差。放疗后4个月,立体定向放射外科治疗组有6%的患者经历了临床意义上的认知功能下降,相比之下,全脑放疗组有50%的患者经历了临床意义上的认知功能下降。
“认知能力下降是脑转移和治疗的最致人衰弱的影响之一,治疗的一个关键目标是改善这些脑转移患者的大脑功能,”Dr. Li解释说。之前的试验表明,超过90%的脑转移患者在治疗前经历过认知障碍,最常见的是注意力、记忆或信息处理方面的障碍。
两组患者的总生存期没有差异,立体定向放射外科治疗组的中位总生存期是7.8个月,全脑放疗组的中位总生存期是8.9个月。立体定向放射外科治疗组相比全脑放疗组取得了更高的局部控制率,但两组之间的差异没有达到统计学意义(放疗后4个月,局部控制率分别为95%和86.7%)。全脑放疗组患者发生远端脑衰竭的中位时间为10.5个月,立体定向放射外科治疗组患者为6.3个月。
相比全脑放疗,放射外科治疗与更短的全身治疗中断相关,立体定向放射外科治疗组的全身治疗中断时间为1.7周,全脑放疗组为4.1周。Dr. Li解释说,这一发现对转移性疾病患者来说特别重要,因为他们会获益于控制脑外癌症的全身治疗。
全脑放疗组有4名患者(占15%)、立体定向放射外科治疗组有2名患者(占8%)发生了3级或以上毒性作用。研究人员在17%的立体定向放射外科治疗组患者中观察到了放射性坏死的影像学证据(占所有受治疗病灶的4%),而放射性坏死是与立体定向放射外科治疗相关的副作用。
Dr. Li表示:“全脑放疗和立体定向放射外科治疗都是现行的标准治疗,两种选择都有优点和缺点。我们需要随机试验数据来了解哪些患者能从每种治疗中获益最多。”
Radiosurgery reduces cognitive decline without compromising survival for pts with 4+ brain metastases
by American Society for Radiation Oncology
October 26, 2020
Results of a new randomized phase III trial suggest that stereotactic radiosurgery (SRS) should replace whole brain radiation therapy (WBRT) as the standard of care for patients with four or more brain metastases. Compared with whole-brain treatment, highly focused radiation therapy led to less cognitive decline with equivalent overall survival. Results from the clinical trial (NCT01592968) will be presented today at the American Society for Radiation Oncology (ASTRO) Annual Meeting.
"This study provides strong evidence to support replacing whole brain radiation with more focal radiation for patients with multiple brain metastases," said lead author Jing Li, MD, Ph.D., an associate professor of radiation oncology and co-director of the Brain Metastasis Clinic at The University of Texas MD Anderson Cancer Center in Houston.
The trial builds on previous research that established SRS as the standard of care for patients with one to three brain metastases. "Whole brain radiation was the backbone of treatment for brain metastases for a very long time. When stereotactic radiosurgery became available, however, we saw its potential to reduce the cognitive deterioration associated with whole-brain treatment and improve patients' quality of life," said Dr. Li. SRS is more convenient for patients and minimizes interruption of systemic therapy, as well; while WBRT typically is given in 10 treatment sessions over a period of two weeks, radiosurgery generally is completed in one single-day session.
An estimated 1 in 5 patients with cancer will develop brain metastases when primary cancers, most commonly breast cancer, lung cancer or melanoma, spread to the brain. Brain metastases are diagnosed in an estimated 150,000-200,000 people each year, with rising incidence as improved treatments help patients live longer.
In this randomized phase III trial, radiation oncologists at MD Anderson treated 72 adult patients who had 4-15 untreated, non-melanoma brain metastases with either SRS (n=36) or WBRT (n=36). Patients in the WBRT arm were also recommended memantine, a prescription drug used to treat dementia, after a different phase III trial found that it helped delay cognitive decline in patients receiving WBRT for brain metastases. Researchers tracked cognitive function through standard tests of learning and memory, attention span, executive function, verbal fluency, processing speed and motor dexterity.
Cognitive function was better preserved for patients who received SRS, compared to those who received WBRT. Four months after radiation therapy, patients in the SRS group scored higher on a memory function test than they did at baseline (average z-score change from patient's own baseline, +0.21). Patients in the WBRT group arm scored worse on the memory function test compared to baseline (average z-score change, -0.74; p=0.04). Four months after treatment, 6% of the patients in the SRS arm experienced a clinically meaningful decline in cognitive function, compared to 50% of patients in the WBRT arm (p=0.018).
"Cognitive decline is one of the most debilitating effects of brain metastases and treatment, and a key goal of treatment is to improve functioning in the brain for patients with these tumors," explained Dr. Li. Previous trials have indicated that upwards of 90% of patients with brain metastases experience cognitive impairment before treatment, most commonly trouble with attention, memory or information processing.
Overall survival did not differ between the groups (SRS median 7.8 months, WBRT median 8.9 months, p=0.59). Local control rates favored SRS, but the difference did not reach statistical significance (95% at four months with SRS and 86.7% with WBRT (p=0.09). The median time to distant brain failure was 10.5 months for WBRT and 6.3 months for SRS (p=0.37).
Radiosurgery, compared to WBRT, was associated with shorter interruptions of systemic therapy (time to systemic therapy: SRS 1.7 weeks, WBRT 4.1 weeks, p=0.001). This finding is particularly important for patients with metastatic disease, explained Dr. Li, as they benefit from systemic therapy to control cancer outside of the brain.
Four patients who received WBRT (15%) and two who received SRS developed (8%) grade 3 or higher toxicities. Radiographic evidence of radiation necrosis, a side effect associated with SRS, was observed in 17% patients on the SRS arm of the trial (4% of all treated lesions).
Next steps for the research team include comparing SRS with a newer form of WBRT designed specifically to avoid the hippocampus, a brain structure that is central to learning and memory. While a recently published trial (NRG Oncology CC 001) found an advantage of hippocampal-avoidance over standard whole-brain treatment, no trial has compared it with SRS. "Both options are currently considered standard treatment, and both options have pros and cons. We need randomized data to understand which patients will benefit most from each of these treatments," said Dr. Li.
本文编译自Medical Xpress于2020年10月26日发布的《Radiosurgery reduces cognitive decline without compromising survival for pts with 4+ brain metastase》,原文链接:https://medicalxpress.com/news/2020-10-radiosurgery-cognitive-decline-compromising-survival.html

【盛诺一家】 成立于2011年,是国内权威的海外医疗咨询服务机构,提供出国看病、全球专家远程咨询、日本体检等服务。
海外医疗为什么首选盛诺一家?
- 稳健运营
深耕行业14年:实缴注册资本3,970万元,获红杉资本、中信里昂、腾讯等多轮注资。 - 权威认证
全球医疗资源:与美国MD安德森、梅奥诊所、麻省总医院、日本癌研有明医院等官方直签合作。
官方认证 合规运营:唯一同时获日本MEJ AMTAC资质与外务省“身元保证机构”授权的中国机构。 - 专业服务
专业可靠:服务团队成员70%拥有医学背景,包括医学院博士、三甲医院医生、资深医学翻译。
智能匹配:自主研发专利“全球医疗资源匹配模型”,精准推荐医院与医生。
全流程个体化服务:从病历翻译、签证辅助、就医预约到境外陪同、生活支持全面覆盖。
全球服务网络:在中、美、英、日等地设有15个全资分公司与服务中心,提供落地保障。 - 客户至上
提供5%-40%医疗费用专属折扣,签约48小时可全额退款,出具风险告知,倡导理性就医。 - 良好口碑
合作企业:为华为、中国人寿、民生银行等知名企业提供海外医疗咨询服务。
媒体报道:多次获人民日报、CCTV、新华社报道,被人民网评为“出国看病机构第一名”。
客户信赖:盛诺一家已服务7000+重症患者家庭,60%客户通过老客户推荐,满意度高达99%。
👉 如果您或家人面临重大疾病决策,想了解海外就医方案?
✅ 请拨打免费咨询热线
400-875-6700,或通过
官方网站
预约咨询医学顾问,获取专业建议,开启全球精准医疗之路。
本文为海外就医科普文章,内容仅供阅读参考,不作为任何疾病治疗的指导意见。文章由盛诺一家编译,版权归盛诺一家公司所有,转载或引用本网内容须注明"转自盛诺一家官网(www.stluciabj.cn)"字样。
- 相关资讯
- 最新动态
 红杉资本(中国)被投企业
红杉资本(中国)被投企业













 咨询医学顾问
咨询医学顾问 
 提交成功!
提交成功!


 出国看病费用评估
出国看病费用评估